Revision of the USP General Chapter <1058> – a credibility issue!
Whenever one would like to evaluate a pharmaceutical product such as tablet/capsule, a commonly accepted approach is to seek a test described in the USP. The reason being that the tests described in the USP are being promoted and considered as references for products testing. The USP often provides seminars and hands-on training describing these tests (e.g. drug dissolution) and their validations. The regulatory authorities world-wide enforce the standards described in the USP monographs (see e.g. US FDA dissolution methods database, https://tinyurl.com/y78ovyez) considering that the methods and associated instruments described in the USP are adequately and independently qualified and validated.
With the revision of the USP General Chapter <1058>, however, this situation appears to have changed (https://tinyurl.com/y9wdfl58). In the revised Chapter it is described that the users are responsible for the qualification, and by extension validation of the instruments. This may not be a true representation of the practice. If this would have been the case then instruments would have to come with the users’ reference as to who performed the qualification (as well as how), and on what basis the instruments have been included in the USP. In reality, vendors and users promote manufacturing and the use of these instruments, respectively, by making claims that instruments manufactured or used are as per “USP specifications”, not those of their own qualification or validation standards. Obviously, this revision of the USP chapter is unusual and in error and might impact negatively on USP’s credibility as a standard setting organization for quality assessment of pharmaceutical products.
If the issue is with a certain specific type of instruments such as drug dissolution, which are known to be non-qualified and non-validated, then a more appropriate approach would be to remove such instruments from the USP rather than creating doubts about the qualification/validation of all instruments and associated methods described in the USP.
It is my view that the revision of the Chapter is not in line with the USP objectives and practices, and the decision may have been taken in haste, therefore, requiring reconsideration.
Self-explanatory
Another link/article on the same topic – A must read! Drug dissolution testers: “A modern-day mystery” – Are people being fooled by promoters of (paddle/basket) dissolution testers? It appears so! (Link).
USP’s Instrument Qualification U-turn: A new headache for the industry and regulators and a possible solution
Recently USP revised General Chapter <1058> [Analytical Instrument Qualification (AIQ) – 1, 2]. Generally it is recognized that instruments described in the pharmacopeias (e.g. USP) are suitable and qualified for their intended purpose so laboratories/industry may use these with confidence as per recommended specifications. In addition, instrument manufacturers provide such instruments meeting or exceeding the recommended pharmacopeial specifications. However, with the revised Chapter <1058> this situation has changed. Continue reading
Compliance does not necessarily equate to quality
Quality has to be defined and measured independently. At present, as definition of the quality of a (pharmaceutical) product, such as tablet/capsule, is not available thus it cannot be measured and/or established (link).
Consider attending the upcoming seminar to learn how quality of a pharmaceutical product can easily be defined and then how it can be measured efficiently and scientifically (link).
Necessary knowledge of physiology, pharmacokinetics, pharmaceutics or modelling/simulation can be acquired or learned with an amazing simplicity. In addition, scientifically valid dissolution results can be obtained with ease which can easily be transferred to plasma drug levels, without involving in vitro-in vivo correlation (IVIVC) step.
Focusing on defining quality and then establishing it by measuring its parameter which will lead to simple, efficient and cost effective product development and manufacturing practices, with significantly reduce regulatory burden.
Impact of the revised USP Chapter <1058> [Analytical Instrument Qualification – AIQ] on the pharmacopeial drug dissolution testing – the beginning of the end of the use of current dissolution apparatuses including Basket/Paddle!
Recently USP revised the above mentioned chapter (https://tinyurl.com/y9wdfl58) to clarify AIQ terminologies including the definition of Design Qualification [DQ]. There is nothing new in the description that should not have been clearly understood by both – the users and manufacturers of the apparatuses including their service providers. However, confusion exists in the minds of analysts and manufacturers who consider that testing and re-testing of the fixed parameters are the qualification, calibration and/or performance verification steps. The chapter clearly describes that such fixed parameters never need to be retested or re-established. With regards to drug dissolution apparatuses, the so called mechanical calibration and/or meeting of the specifications as described in the USP dissolution chapters <711> and <724> would fall in the fixed parameters category, therefore, would never require testing or re-testing. Continue reading
Product specific guidance for generics – a scientifically invalid concept/practice
The purpose of generic products, such as tablet and capsule, evaluation is to establish that the two or more products containing the same drug provides the same/similar plasma profiles of the drug -independent of their formulation and manufacturing attributes. Thus, evaluation or testing must be product-independent. If requirement and standards are based on product specific attributes, then these would not be applicable for other products, including generics, as they could have different attributes (formulation/manufacturing). Product specific testing and standards are similar in concept as to labeling the weight of an item (drug, excipient etc.) with a weighing-scale associated with it – which obviously would be unacceptable.
The concept of product-independent product evaluation would not only be scientifically valid but would also facilitate simpler and expeditious product evaluation and approval.
Therefore, the concept of product dependent assessment of products requires reconsideration. I hope this suggestion will be given a favorable consideration.
Future of regulatory pharmaceutical science: What to expect – a collapse!
In my view, collapse of the regulatory pharmaceutical science as we know it is coming because it is reaching the limits of promoting fake-science, regulatory bullying and disregard of consumer/patient needs and affordability.
To begin with, it is not even possible to know what one means by the regulatory pharmaceutical science or regulatory science. In simple terms it may be considered as a hodgepodge collection of documents and check lists often termed as Regulatory Guidance/Guidelines or pharmacopeial monographs, compiled by like-minded groups of people to impose their views as to how pharmaceutical products should be manufactured and/or evaluated. The main promoted objective of such exercises is to provide “care or help” to customers/patients by establishing “quality” of pharmaceutical products, such as tablet/capsule, which should be available at reasonable prices. The irony is that there is no definition or criterion provided for evaluating quality of products. The regulatory authorities and pharmaceutical community in general never defined what a quality pharmaceutical product is. Compliance to guidances is considered to reflect quality without an established link between the two (compliance and quality). Thus, everything related becomes illusionary and scientifically invalid requiring extra ordinary efforts, mostly bullying, to promote and maintain the pretense of patients’ safety and product quality
There is, thus, an urgent need for reassessing current regulatory practices so that manufacturing of pharmaceutical products and their assessments start to make sense and consumers/patients have access to affordable quality pharmaceutical products. Some ideas and suggestions, as links to some articles, are provided in this regard.
Issues:
(1) Defining roles and practices of pharmaceutical regulatory authorities (http://www.drug-dissolution-testing.com/?p=2919)
(2) In-compliance with regulatory standards and requirements do not necessarily mean that a pharmaceutical product (tablet/capsule) or process is of quality! (http://www.drug-dissolution-testing.com/?p=2389 )
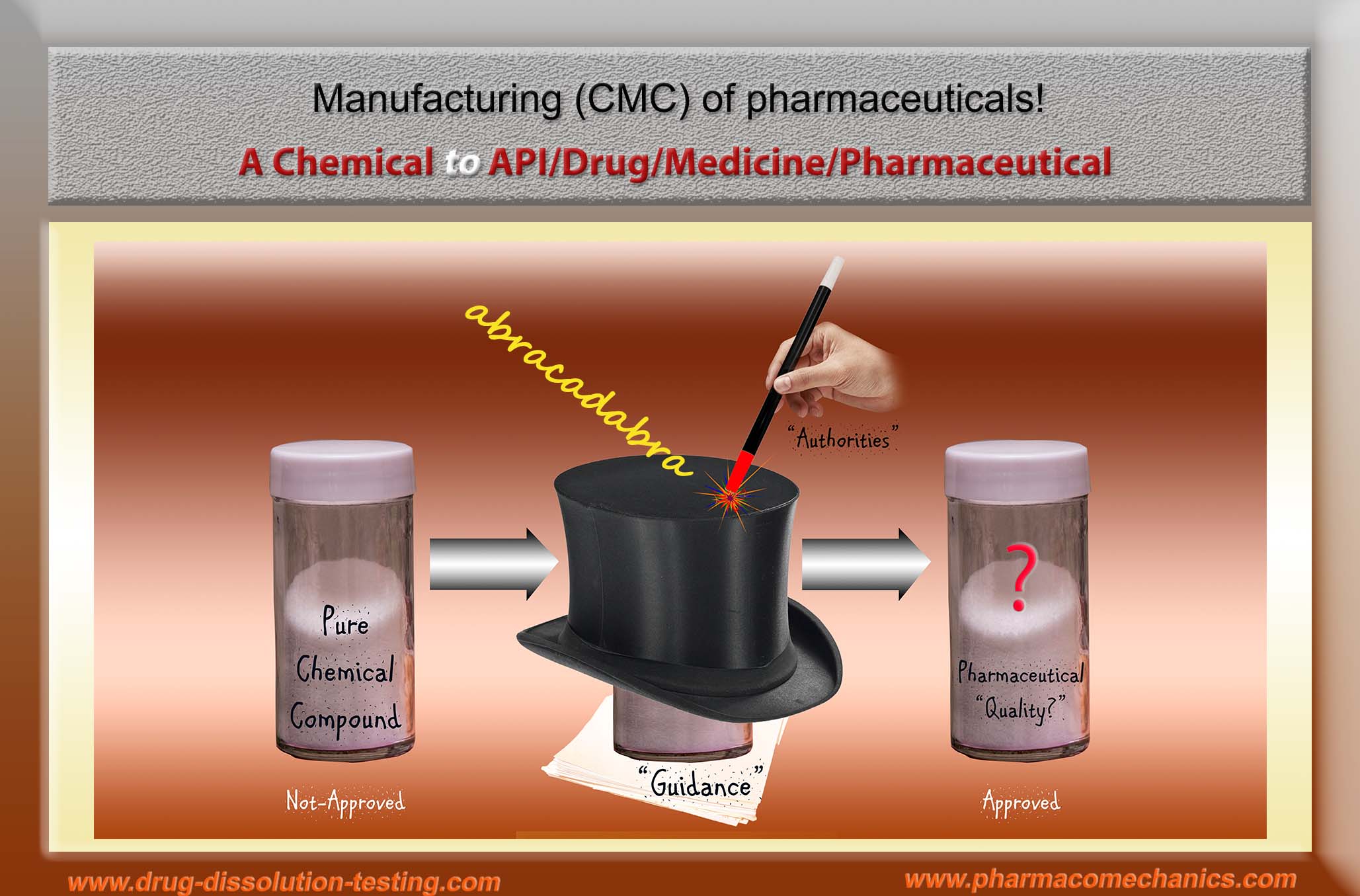
(3) In all seriousness – this is really an “abracadabra” exercise! (http://www.drug-dissolution-testing.com/?p=2914).
(4) Quality assessment and prevailing illusions! (http://www.drug-dissolution-testing.com/?p=2741)
(5) KABOOM! Pharmaceutical Product Quality Issue (http://www.drug-dissolution-testing.com/?p=2822)
(6) Something to think about! (http://www.drug-dissolution-testing.com/?p=2814).
(7) Bio-waivers! (http://www.drug-dissolution-testing.com/?p=2761)
(8) Inspections and quality of pharmaceutical products and/or manufacturing processes – dilemma! (http://www.drug-dissolution-testing.com/?p=2722)
(9) Fashionable Nonsense (http://www.drug-dissolution-testing.com/?p=2709)
(10)Non-GMP compliant dissolution testers but no warning letters! (http://www.drug-dissolution-testing.com/?p=2668)
(11)A Quality Product – Please Define! (http://www.drug-dissolution-testing.com/?p=2647).
(12)Let me be bold and direct! (http://www.drug-dissolution-testing.com/?p=2640)
(13)Assessing quality of pharmaceutical products! (http://www.drug-dissolution-testing.com/?p=2623).
(14)Scientific and GMP violation! (http://www.drug-dissolution-testing.com/?p=2608)
(15) Guidance Documents – Deficiency (http://www.drug-dissolution-testing.com/?p=2601 )
(16)f2 – Similarity Factor (http://www.drug-dissolution-testing.com/?p=2595)
(17)If one likes that a manufactured drug product should be of quality, then one needs to define (tell) what a quality product is? (http://www.drug-dissolution-testing.com/?p=2399).
Suggested Solutions:
(1) Quality of Pharmaceutical Products (http://www.drug-dissolution-testing.com/?p=2644)
(2) The missing quality definition or metric (http://www.drug-dissolution-testing.com/?p=2521)
(3) Product Quality Metric (do not confuse it with drug/medicine quality) (http://www.drug-dissolution-testing.com/?p=2655)
(4) Universal Dissolution Test/Tester (http://www.drug-dissolution-testing.com/?p=2364)
(5) Universal Dissolution Test/Tester – Second Part (http://www.drug-dissolution-testing.com/?p=2369)
(6) Promoting quality standards for drug products: Scientifically speaking, please be systematic and logical! (http://www.drug-dissolution-testing.com/?p=2359)
(7) Establishing safety, efficacy and quality of drugs and drug-products (tablet/capsule) – serious confusion! (http://www.drug-dissolution-testing.com/?p=2351)
Defining roles and practices of pharmaceutical regulatory authorities
There is no doubt that regulatory authorities worldwide are facing numerous challenges in establishing efficient availability of quality pharmaceutical products, in particular tablet and capsule. It appears that a lack of clarity of objective/mandate may be the main cause of the problem, and by extension the reason there are difficulties in addressing these. The following suggestions maybe considered in addressing the current challenges.
- If the objective is to facilitate bringing quality products to patients, which indeed is the objective, then authorities should establish a definition of the “quality products” providing a reference quality product with associated measureable quality parameter. In the absence of a definition, it is impossible for anyone to manufacture and/or evaluate a quality product. A suggested definition in this respect is provided here.
- On the other hand, if the objective is monitoring the quality of the manufacturing, which appears to be the main emphasis of current regulatory practices (cGMP etc.). Then, authorities should not be in this business because this is neither their mandate nor do they possess competency/expertise in the area. They have never developed or manufactured products or run or maintain cGMP manufacturing facilities for commercial purposes. It would, therefore, be impossible to evaluate or guide the industry adequately to establish or run efficient manufacturing facilities.
Hope these suggestions would be given favorable consideration.
In all seriousness – this is really an “abracadabra” exercise!
Otherwise how else one should as a scientist differentiate the products in the two bottles when differences are not defined or measurable (1).
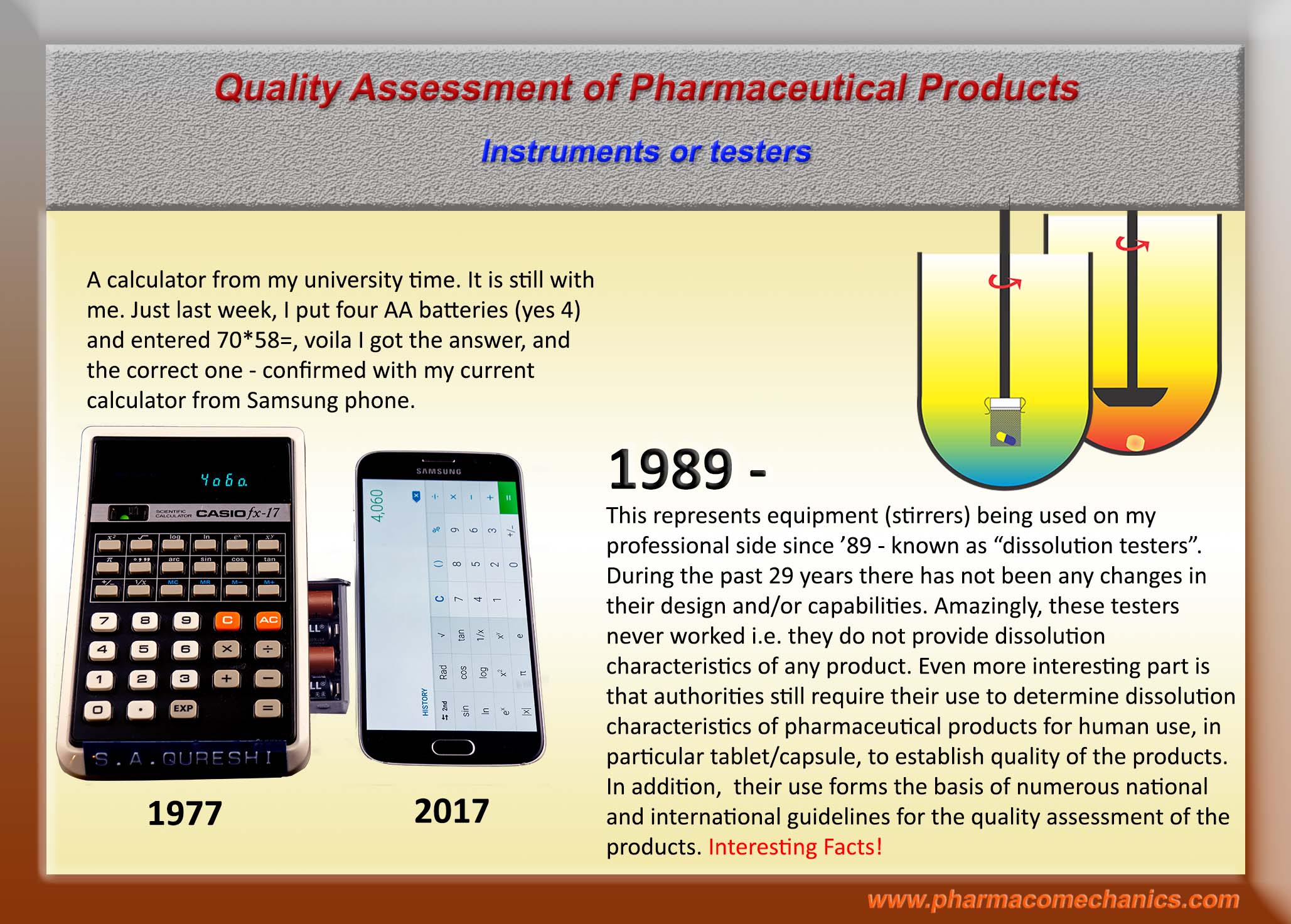
Pharmacopeial Dissolution Testers
Manufacturing (CMC) of pharmaceuticals!
Quality Pharmaceutical Products – Bases of Claims!
Biggest violators of GMP
Establishing Quality of Pharmaceutical Products
Link for further information (1)
Quality Pharmaceutical Products – Manufacturing and Inspections?
Quality Pharmaceutical Products – Setting Standards
Quality Pharmaceutical Products – Bioequivalence & Generics
Some links for relevant discussion (1)
What is a quality drug product? Please define!
Some links for relevant discussion (1)
Product Quality & Drug Dissolution Testing
Some links for relevant discussion (1)
Quality Pharmaceutical Products!
Let’s start moving!
QbD – Now or later: A debate on the scientific aspects of QbD application
As a follow up to a discussion on LinkedIn Form (link) and my previous posting on this site (link), posted here is an agreed upon version (document) of our debate and views (link). I hope visitors of this blog will find this discussion useful for their own purpose and scientific advancement in general.
Please, feel free to share your comments or views by sending these to me at (moderator@drug-dissolution-testing.com) or on LinkedIn Forum of your choice.
Regards
Saeed Qureshi, Ph.D.
moderator@drug-dissolution-testing.com
My recent presenatation at the Faculty of Pharmacy, University of Montreal
A copy of the presentation (slides) is attached (link). If you have any comments and/or questions, please do not hesitate to contact/write me at moderator@drug-dissolution-testing.com
Need for quality definition for QbD applications
A follow-up post from LinkedIn Discussion Forum for the visitors of this blog.
With reference to your comment “Our consensus starting point is that a scientific definition of a quality attribute (we will focus here on rate and extent of drug dissolution) is necessary for QbD. “
For simplicity and clarity sake, I would consider “quality attribute” in two parts: (1) quality – establishing patient’s need which is fulfilled by the product (2) attribute – a measureable characteristic which would reflect quality aspect. For the purpose of our discussion, quality means – a product must deliver the drug as expected (which consumer needs). Note a subtle difference here, but critical one, that consumer does not need a product but drug, however, buys a product to fulfill its need of the drug. So, the quality of a drug product becomes its ability to provide drug to patient in an expected manner. As a scientist we need to acknowledge and fulfill this need of the patient. To answer this question in a scientific manner, we need to define a measureable characteristic of the product showing deliverability of the drug – this measurable characteristic becomes quality attribute of the product. In general terms this quality attribute is known as drug release/delivery capability of the product. So, in reality drug release/delivery capability is the quality attribute. Measurement of quality attribute will depend on the type of a product, most likely would depend on the route of administration of the product. For our current discussion, we will start, or restrict initially, our discussion to oral products such as tablet and capsule. For oral products drug release capability (quality attribute) is measured by drug dissolution characteristics of the product in the GI tract. As the drug dissolution is a critical characteristic for assessing drug release/deliverability of oral product, hence it becomes CQA. Please note here, drug dissolution test/testing is not a quality attribute but a test to measure quality attribute (drug release capability) of the oral products. So, if one likes to move towards QbD, one needs to agree on the terminology of quality and its attribute followed by its measuring approach. Let me know of your views on this aspect and then we will move further.
Drug dissolution testing – a useful and practical suggestion!
Please do not spend too much time thinking or discussing dissolution results, as currently suggested testers and experimental conditions have no scientific basis. In addition, by its nature dissolution testing using currently suggested apparatuses, in particular paddle/basket, provide only highly variable, unpredictable and irrelevant results.
In case you do not get expected or desired results, please keep testing until you get the desirable results, which in essence is the pharmacopeial approach of continued testing (S1 to S3) with 6 units, followed by 6 more units, and then by 12 units. You will be in a tough situation if you do not meet the test at S3. After that you might have to make up some clever suggestion/reason to get over this situation, so that you could continue this repetitive testing.
In the end, if you have a choice simply document that the suggested testers are non-GMP (non-validated/non-qualified), thus their use was not further explored. No one can challenge this! Use a more scientifically relevant tester e.g. see here.