Are people using drug dissolution testing for product development? Not really!
Title of the post is a bit catchy, but is factually 100% correct, i.e. no one is using dissolution testing for product development, as explained below:
Suppose a formulator would like to develop a product having a certain dissolution characteristic/profile. The product is to be developed for human use; therefore, the target dissolution characteristic/profile should be relevant to humans as well. With this objective in mind, the formulator proceeds to developing a product by mixing some ingredients/excipients and compressing it into tablets, referred to as product “A”. However, the formulator realizes that perhaps all he/she is required to do is to compress the pure drug (powder) into tablets which might give the desired dissolution characteristic. So, he/she compresses the drug powder into tablets as well, referred to as product “B”. Now the formulator would like to determine/compare dissolution characteristics of these tablets, i.e. if they are able to provide the desirable characteristics or require some adjustments. For this purpose, the formulator requires a dissolution test/method (apparatus and associated experimental conditions). Unfortunately, currently no such test/method exists. Therefore, a formulator cannot determine dissolution characteristics of the products, and thus cannot develop a product having a desired characteristic. Continue reading
Drug dissolution testers – reality!
USP General Chapter <1092> Dissolution Procedure: Development and Validation. Perhaps the major reason for the distorted science of drug dissolution testing
This chapter appears quite popular and is often cited as a source for help and information concerning dissolution methods development and validation. However, if one evaluates it, even superficially, one should immediately realize that the chapter is based on invalid assumptions and false science. For example:
The chapter is meant to be helpful and useful in developing and validating a dissolution method. However, the problem is that for such a purpose a fundamental requirement is that one requires a reference product with known dissolution characteristics established independently. In this case, one requires a reference product, which should be approved for human use as the method is to be used for such a purpose, with known dissolution characteristics. The (dissolution) method development means that, using valid scientific principles and testers, the developed and validated method would be able to provide an expected answer for the reference product. This developed and validated method will then be used for evaluating the test products. As, at present, a reference product with known dissolution characteristics is not available, therefore, it is not possible to develop and validate a dissolution method. It is simply a scientific impossibility.
Furthermore, the valid scientific principles and testers mean that developed and validated method must be based on experimental conditions which are relevant to applications of the method. In this case, the relevancy aspect comes from the physiological environment of the GI tract in particular intestinal. The only purpose of the test/method is to evaluate dissolution characteristics of a drug product in the GI tract. It is important to note that even for QC purposes the method measures the dissolution characteristics for the GI tract that is why most, if not all, pharmacopeial tests are conducted using physiologically relevant conditions as well. Therefore, the choice of experimental conditions must be physiologically relevant.
A basic or fundamental requirement, in this regard, is that whatever experimental conditions one chooses to represent the GI tract environment, these should remain consistent from product to product or should be product independent, as does the GI tract environment. This is the second flaw (invalid science) of this chapter that it suggests and emphasizes selecting the test product dependent experimental conditions. It will be impossible to determine true and accurate dissolution characteristics of a test product using experimental conditions specific to the product itself. Furthermore, as the experimental conditions change from product to product, which is unlike the GI tract environment, therefore, such tests would be considered invalid for any purpose. No matter how one presents the argument, for product dependent experimental conditions, it will be an irrelevant evaluation method and test.
It is, therefore, critical to understand that the chapter cannot provide help or accurate information for developing or validating a scientifically valid dissolution method.
Apparatus dependent dissolution/product characterization – a serious misconception and scientifically invalid practice
It is often suggested that to obtain appropriate dissolution characteristics of a product one may use or select an apparatus depending on the product attributes and/or desired release characteristics such as discriminating profiles, reproducibility, bio-relevancy etc. Such reasoning however, dictates that the analyst/formulator should have an idea about the expected outcome of the results, whether based on an educated guess or from prior experimentation. By selecting a particular apparatus and/or its associated experimental conditions, one is in fact trying to achieve the results reflecting one’s own expectation.
For example, when one conducts an experiment using the paddle apparatus and finds dissolution results of a tablet product, and their variability, higher than expected while observing that some, or all, tablets are floating within the vessel during testing. Such behavior or experiment is commonly considered flawed or inappropriate. A common practice to rectify this “problem” is to either use the basket apparatus, or a sinker, to restrict this floating behavior assuming that this may be causing the higher results and variability. This means that the analyst/formulator already has a preconceived idea/expectation about the results and variability of the product, and is trying to obtain those results by adjusting the means, in this case by using a different apparatus or a sinker. Obviously, the analyst is not determining dissolution characteristics of the product but achieving intended results by adjusting tester and/or associated experimental conditions. Continue reading
In reality, and for all practical purposes, pharmacopeial dissolution testing should be considered as bio-waivers! Suggesting otherwise simply confuses reality and science.
Similar C-t (plasma drug concentration-time) profiles or BA/BE (bioavailability/bioequivalence) shows that the products (tablets/capsules) provide similar dissolution characteristics (all other things being equal). Therefore, for all practical purposes the C-t profiles or BA/BE studies are the measure of in vivo dissolution characteristics of the products. Thus, by definition, assessment of in vivo dissolution becomes a product assessment/development tool while the same assessment tool becomes a quality control/assurance tool as well. It is scientifically and logically incorrect to separate or differentiate dissolution tests on the basis of their use, i.e. as a product assessment/development tool and a “quality” control/assurance tool. The dissolution test remains exactly the same in both cases.
The same BA/BE test can be, and are, used during the product development stage as well as for comparing the performance of different batches of the same product. The BA/BE test does not change with the stages of product development and manufacturing.
Considering ethical reasons (testing in humans), cost and time, BA/BE tests can neither be conducted, nor conducted routinely, but only for confirmatory purposes. However, for all other purposes such assessments (during product development stage and as a quality control tool during manufacturing of products) dissolution characteristics of a product are evaluated by in vitro dissolution tests. For all practical purposes current drug dissolution tests are indeed used as a substitute of BA/BE, including for QC purposes such as pharmacopeial tests. Therefore, by definition dissolution tests conducted as recommended, are indeed bio-waivers. One does not require any further or special step to transfer a dissolution test to a bio-waiver status or vice versa. Stating otherwise would not change the reality or the fact.
If a dissolution test does not provide an in vivo relevant outcome, then the issue is with the dissolution test and such a test should not be used any further until corrected. Requiring the use of dissolution tests which do not provide bio-relevant results, for any purpose, cannot be justified on any basis, scientific or logical. It simply confuses reality, science and people, and furthermore hinders efficient product development and manufacturing.
Drug dissolution testers: “A modern-day mystery” – Are people being fooled by promoters of (paddle/basket) dissolution testers? It appears so!
Struggling with developing or evaluating tablet/capsule products/formulations? The following considerations should be helpful
A drug dissolution test is one of the most critical and important tests used for developing and evaluating tablet/capsule products. However, unfortunately, as conducted at present the test is also perhaps one of the most frustrating and the least value adding tests one would use. The test is often promoted as a quality control test or tool as well, however, without defining or linking to a quality parameter/end-point. It is conducted using apparatuses which have never been validated for the intended purpose or objective, which further adds to the frustration. This article describes reasons for such practices and frustrations, and suggests a simple approach to address the issues and concerns.
Please click here for complete article
“USP General Chapter <1092> The Dissolution Procedure: Development and Validation”: Comments on proposed revisions
USP is seeking comments on a draft of the revised “General Chapter <1092> The Dissolution Procedure: Development and Validation” (link). Also provided is a Stimuli article: “Revision of <1092> The Dissolution Procedure: Development and Validation” (link), which is to be published along with the proposed General Chapter providing the background information for the suggested revisions.
The following provides some comments for the consideration of the USP:
(1) In general, the chapter appears poorly written lacking focus and coherence of thoughts.
(2) The claims made in the article, for method development or validation, are not only vaguely described but are also scientifically invalid. For example:
- The suggested apparatuses, in particular paddle/basket, are known to be flawed (lack reproducibility and relevancy) and have never been validated. Therefore, developing or validating a method using such apparatuses would not be possible.
- For validating a method, one requires a reference such as a product, parameter value (e.g. dissolution results) and/or experimental conditions established independently. As such a reference is not available at present, thus the dissolution methods cannot be developed in particular for setting regulatory/pharmacopeial standards such as for USP.
- The suggested approach of method development appears to be a vague narration of selecting experimental conditions to obtain certain pre-defined or pre-conceived dissolution characteristics of a product, not for determining the true characteristics of a product. It is important to note that the choice of the experimental conditions should be linked to the GI tract environment and not the product. As the physiological conditions (or experimental conditions) remain constant or independent of the drug/product, one should not be able to vary experimental conditions. The suggestions in the chapter concerning selecting product-dependent experimental conditions are scientifically invalid for the purpose.
- In general, if given a blinded product sample, which is a normal and common analytical practice, no matter how thoroughly or attentively one would follow the suggestions provided in the chapter it would not be possible to determine relevant and/or true dissolution characteristics of any product.
USP should consider addressing the above mentioned deficiencies before finalizing the chapter.
Interpreting dissolution results, an exercise in futility
The most commonly reported results from dissolution testing for establishing the performance of oral products (e.g. tablets/capsules), in particular for immediate-release (IR) products, is that products should meet a criterion of not less than 80% drug dissolution within less than 60 minutes, mostly 30 minutes.
Let us assume that a dissolution test (n=6) provides the following results (% drug dissolved) at 30 minutes (96, 88, 65, 110, 66, 65; Ave = 82; RSD = 23%). Obviously, this test/product, with at Q of 80%, would not meet the USP tolerance at the first stage. However, with a bit of luck and a second round of testing of 6 units it may meet/pass the USP Tolerance criteria. For details, please see the link, in particular the data set in row one.
Let us discuss the interpretation of these observed results. Continue reading
Are low solubility drugs really problematic? Maybe not!
Drug absorption from the GI tract is generally dependent on dissolution characteristics of a product which in turn is dependent on the aqueous solubility of the drug. In general, it is assumed that the higher the solubility, the higher the expected drug absorption will be, and vice versa.
Before considering the link between absorption and solubility, it should be prudent to define and establish the solubility characteristics of a drug for absorption purposes. In this regard, it is a well-known fact that drugs are mostly absorbed from the intestinal part of the GI tract (link). The liquid phase in the intestine is aqueous-based having a pH in the range of 5 to 7. For all practical purposes one may consider a pH of 6 (average of 5 to 7) for the intestinal fluid. Thus, to represent intestinal fluid, for dissolution testing, one may use water itself, which usually has pH around 6 or a (phosphate) buffer having a pH of 6. Therefore, in the following discussion, solubility of drugs in water will only be considered.
Permeability, absorption, and bioavailability of a drug and drug dissolution testing
The quality of a solid oral dosage form, such as a tablet or capsule product, may be defined as its ability to provide expected and consistent (reproducible) drug levels in plasma/blood. The product is introduced into the GI tract through the oral cavity (mouth) to release its drug, which gets dissolved in the aqueous milieu and gets transferred into the blood stream to produce its therapeutic effects.
This transfer of a drug from the GI tract to the blood stream is described by different terminologies, often interchangeably, such as permeability, absorption and bioavailability of the drug. However, these terminologies have distinct meanings, and for clarity purposes should not be interchangeably used. The purpose of this article is to describe and explain these terminologies to facilitate an appropriate development and evaluation of the products in particular for the use of in vitro drug dissolution testing. Please click here for complete article
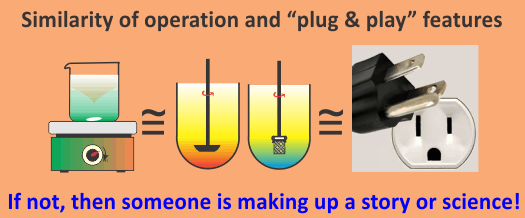
Drug dissolution testing for product development: An easy and simple approach
At the product development stage the objective is to develop a product (tablet/capsule) having certain desired drug release/dissolution characteristics in humans. Therefore, one requires a dissolution method mimicking in vivo or the GI tract environment (in particular that of the intestinal). Commonly, this in vivo environment for dissolution testing purposes is represented by three variants: (i) temperature (37 ºC); (ii) an aqueous based solvent/medium; (iii) a container or vessel with a stirrer to provide interaction between product and solvent.
Another requirement, which is perhaps the most critical one and is often overlooked, is that the method or testing environment must also be product independent as does the GI tract environment.
It is further important to note that the method to be used must have already been developed and validated independently of the product which is underdevelopment. On the other hand, it is a common practice that people use or develop product dependent dissolution methods. However, unfortunately such a practice is neither scientifically valid nor correct. Furthermore, the use of a product dependent method cannot provide true or actual dissolution characteristics of the product (link).
At present, none of the commonly suggested/recommended testers/methods, including pharmacopeial, provide common and/or product independent methods or experimental conditions. Thus such tests/methods cannot provide scientifically valid and/or true dissolution characteristics of a product during the product development stage.
This present day limitation can easily be addressed with the use of the crescent-shape spindle set at 25 rpm with 900 mL of water maintained at 37 ºC. A small amount solubilizer may be added to water/medium if the drug is of low aqueous solubility. For more details regarding advantages of using crescent-shape spindle please follow the link.
Seeking Metrics to Define Drug Quality
As a part of a discussion (link) on the LinkedIn Network group (Quality-by-Design), I posted the following response. For the interest of people who do not participate in the LinkedIn Network or the particular group, I am posting the response on the blog as well. I hope that you will find the post useful.
I think it is a critical and very important topic (FDA Seeks Metrics to Define Drug Quality, link) i.e. defining metric(s) for establishing “quality” of pharmaceutical products. This has also been my view, and it has been stated on this forum a few times as well, that one cannot determine, monitor and/or improve “quality” of a drug product until it is clearly defined (for example, see links, 1, 2). That is, what is a “quality product” and what parameter should be measured to reflect this “quality”.
My interest/expertise lies in the area of solid oral dosage forms (e.g. tablet/capsule products), where the “quality” of a product may be defined as achieving expected and consistent levels of drug in blood/plasma or body. Therefore, assessing plasma drug concentration-time profiles (aka bioavailability/bioequivalence) becomes a “quality” metric for solid oral dosage forms.
However, because of ethical, time and financial reasons/constraints this parameter cannot be used on a routine basis for manufacturing purposes. Therefore, an in vitro surrogate of concentration-time profiles is required. Drug dissolution testing is that surrogate, with very valid scientific reasons, and has been in use precisely for this purpose for many years.
The most unfortunate and ironic part is that the test itself is scientifically valid, however, the way testing has been done, or required to be done by standard setting organizations, is scientifically and logically invalid and useless. There are at least two reasons which make the current practices invalid: (1) persistent requirement of using dissolution apparatuses/testers which have never been validated for dissolution testing purposes. In fact, suggested/recommended testers, in particular paddle/basket, are flawed and are incapable of providing dissolution results of any product (link); (2) most, if not all, dissolution methods are product dependent, thus cannot provide unbiased or “true” dissolution characteristics of the products (link).
Using a slightly modified dissolution tester along with a suggested simpler method development approach can resolve such issues and would help in defining and monitoring the needed “quality” metric for the solid oral dosage forms (link).
(Pharmacopeial) dissolution tests lack relevance and scientific rationale
An in vitro drug dissolution test is conducted to assess in vivo dissolution characteristics of products usually tablets and capsules. The reason or logic behind conducting this test is that if a drug is to exert its therapeutic effect after administration, it should be absorbed from the GI tract (mostly small intestine). Further, for a drug to be absorbed it should be available in dissolved (solution) form in the GI tract. Thus, measurement of the dissolution of a drug in the GI tract becomes one of the most critical steps for establishing and/or monitoring the efficacy and quality of the drug or its product.
Usually it is not possible that the in vivo dissolution of a drug be monitored directly. Therefore, it is monitored indirectly by measuring bioavailability of the drug, which is estimated from the drug concentrations in the blood or plasma, commonly known as plasma drug concentration-time profiles. On the other hand, as the in vitro dissolution test is used to evaluate in vivo dissolution which is monitored by bioavailability, the in vitro test dissolution test and bioavailability assessment thus becomes interlinked with each other.
It is very important to note that the only purpose or use of drug dissolution testing is to assess bioavailability of a drug from its product, which then reflects the quality of the product. It is also equally important to note that the link between dissolution testing and the quality of the product is through bioavailability assessment only. Otherwise, dissolution testing has no link to the quality of the product or its assessment. Often, it is promoted that dissolution testing is used and/or valuable for monitoring manufacturing efficiency/quality or its consistency. However, unfortunately, this is simply a false description or promotion of dissolution testing. A dissolution test has no ability to monitor anything but dissolution characteristics of a product, which then is used for bioavailability assessment.
It is now also well accepted that the current practices of dissolution testing have not been successful in predicting bioavailability assessment. Recently USP clearly described this situation by including the following statement in one of its general chapters, i.e. “Compliance with any of the [dissolution] tests does not assure bioequivalence or bioavailability” (link).
Obviously, it is clear that dissolution testing cannot be used for bioavailability assessment. What then is the purpose of such (pharmacopeial) dissolution tests? The answer is not much.
On the other hand, if one would address well known deficiencies of the currently suggested dissolution testers/apparatuses, in particular paddle/basket, then not only can dissolution testing be made bio-relevant, but also be vastly simplified and improved.
A modified apparatus/procedure has been suggested using the crescent-shape spindle, with a single set of experimental conditions, to address the above mentioned deficiencies. For further details in this regard, please follow the link.
Dissolution method development practices – reality
In simple terms current practices of dissolution method development may be described as:
“A practice of selecting experimental conditions (e.g. apparatus, rpm, medium) to achieve or observe expected or perceived dissolution characteristics of a product.”
The selected methods (i.e. experimental conditions) are then “labelled” differently at one’s own choosing such as the QC-method, bio-relevant method, discriminatory method, etc. There are absolutely no differences in such methods and/or in their development approaches.
It is important to note that one never determines or establishes dissolution characteristics of any product, one just selects experimental conditions to achieve certain desired results. Therefore, one can never determine/establish quality, for QC, or bio-relevance (IVIVC, bio-waiver, product development etc.) for product development purposes. It has all been a serious and unfortunate marketing illusion.
Moreover, all the suggested or recommended apparatuses, e.g. compendial, have never been qualified and/or validated for dissolution testing purposes, for both bio-relevancy and/or manufacturing links. Therefore, dissolution results commonly obtained using these apparatuses, in particular using basket/paddle, are no different or better than those one may obtain using desk-top blenders, shakers, mixers etc. The point being that at present all the dissolution results, and their interpretations, reported have no meaning, use and/or relevance.
Considering the limitations of current practices, a new and very simple approach has been suggested which addresses issues described above. Further information in this regard can be obtained by visiting the site/blog (link).
Comments on a recently published (review) article
I have had the opportunity to read the (review) article, titled
“In vitro models for the prediction of in vivo performance of oral dosage forms (2013), link”
and certainly it is quite (very) long article, but is it useful? In one way it might be, since it implies that the practices of dissolution testing have not been successful, at least from the in vivo perspective. It is claimed that for QC purposes, the practices may be successful (however, without going into details, I would argue against this view, see below).
My biggest surprise, a pleasant one, is that there is no or limited emphasis on the IVIVC aspect. I am assuming that lack of use or relevance of IVIVC for predictability of plasma drug levels has been recognised. This is great!
On the other hand, there is an emphasis on PBPK (physiologically based pharmacokinetics) modelling (perhaps starting of a new “fad”), with an underlying assumption that one requires complex instrumentation and mathematical modelling to predict plasma drug levels. In my view, such an approach may not be necessary as a simple convolution approach can predict plasma drug levels very well and easily.
Surprisingly (or perhaps not surprisingly), there is no mention of crescent shape spindle, convolution technique or the name Qureshi in the publication. This may reflect lack of credibility of the publication for the literature assessment/review.
In addition, in my view, the publication does not provide any suggestion as to how one should determine dissolution characteristics of a, or any, product (IR or ER). So, the question remains, if one cannot determine dissolution characteristics of a product (e.g. see link), one cannot move further, may it be for QC, PBPK modelling or prediction of plasma drug levels etc.
However, answers to such questions can easily be found as described in the following articles:
(1) Determining blood concentration-time (C-t) profiles from in vitro dissolution results and product evaluation – carbamazepine (link).
(2) A Simple and Unique Approach for Developing and Evaluating Products (link).
Potentially unrealized implication of the recent USP statement “Compliance with any of the [dissolution] tests does not assure bioequivalence or bioavailability”
In a recent addition to USP 37 GENERAL NOTICES AND REQUIREMENTS (link), USP describe that:
“Compliance with any of the [dissolution] tests does not assure bioequivalence or bioavailability”.
The above mentioned statement clearly indicates, or establishes, the fact that compendial (USP) tests and, by extension hundreds and hundreds of similar tests reported in literature, cannot provide in vivo or bio-relevant results.
It is also important and/or critical to note that in most cases there are no differences between methods suggested in compendia and what the manufacturers use during product development stages. In fact, it is commonly suggested and recommended that one should preferably follow the compendial suggested methods as a first choice. Point being, in reality, there are no differences between methods/testers whether they are used for compendial or bio-assessment purposes. Therefore, if compendial methods cannot assure BE/BA then the same methods/testers cannot assure BE/BA in other situations as well, such as for the purpose of product development, bio-waiver, IVIVC etc.
It appears that people are not realizing a potentially profound implication of this statement or view. Some even believe, and are promoting, that it is simply a clarification or “stating the obvious or of already known”. However, in my view, such an interpretation is incorrect. By stating and establishing that compendial dissolution tests do not assure BE/BA, it has clearly challenged all the regulatory guidances and requirements where dissolution tests are recommended for assessing BE/BA. In fact, in my view again, the statement and view has practically made related guidances useless.
Therefore, it is not a simple “stating the obvious or of already known” scenario. It is a profound development which people have not yet realized. However, I believe, it is good and positive news concerning dissolution testing, i.e. by acknowledging the flaws of current practices, USP has opened the door for discussions in seeking modifications and improvements for dissolution testing.
Can the currently suggested compendial dissolution tests be considered as QC-tests? Not really!
In a recent addition to USP 37 General Notices and Requirements (link), USP clearly describes that:
“Compliance with any of the [dissolution] tests does not assure bioequivalence or bioavailability”.
The reality is that dissolution testing has been introduced as an alternative to bioequivalence (BE) or bioavailability (BA) evaluations based on the principle that the dissolution is one of the most critical parameters for the assessment of BE/BA. Drug dissolution tests are, therefore, required to be conducted using physiologically relevant experimental conditions such as 37 ºC temperature, aqueous buffers within physiological pH range, moderate stirring etc.
There has been tremendous effort made in predicting BE and BA (e.g. predicting plasma drug concentration) using testers and methods commonly suggested in the compendia. Dissolution tests have been recommended for bio-waivers i.e. using them in lieu of BE/BA. In addition, it is a common practice and requirement that prior to a test becoming a compendial method the product development step must use, or at least be tried, testers and methods to establish their relevance to BE/BA data. Eventually, the selected dissolution method would become the pharmacopeial test commonly known as QC-test or tool.
The underlying assumption for conducting the test remains that the test monitors potential in vivo dissolution, hence BE/BA. USP Chapter <1092> highlights and stresses that method development exercises should be relevant to in vivo performance describing “The procedure should be appropriately discriminating, capable of distinguishing significant changes in a composition or manufacturing process that might be expected to affect in vivo performance.” Numerous guidance documents, including those from the FDA, stress the dissolution and BE/BA link. Some of the examples to this effect from the FDA guidance’s are reported at the bottom of this post as an appendix.
Therefore, the recent addition to the USP, as noted above, does not make sense. Continue reading
“Compliance with any of the [dissolution] tests does not assure bioequivalence or bioavailability”. The statement has recently been included in USP 37. The question is then, which characteristic/parameter do the tests reflect, and how?
In a recent posting on the USP site, under the heading of (USP–NF General Notices; Updated: 08–Aug–2013) it is stated that the following text will be added to the USP 37 GENERAL NOTICES AND REQUIREMENTS (http://www.usp.org/sites/default/files/usp_pdf/EN/USPNF/revisions/2013-07-09_general_notices_usp37-nf32_final.pdf (link not working) [try this one]
“4.10.11. Dissolution, Disintegration, and Drug Release Tests
Multiple Dissolution, Disintegration, or Drug Release tests may be present in the monograph. The order in which the tests are listed in the monograph is based on the order in which they are approved by the relevant Expert Committee for inclusion in the monograph. Test 1 is not necessarily the test for the innovator or for the reference product. Compliance with any of the tests does not assure bioequivalence or bioavailability” [emphasis is mine].
So what good are these testers/methods then? Furthermore, if their use is to be continued as usual then one requires knowing which characteristic/parameter of the product these compendial dissolution tests are measuring and how. In addition, some supporting evidence should also be provided showing how the current dissolution testers/methods have been qualified and validated for the suggested characteristic/parameter. Continue reading
F2 (similarity factor) or a 2F (faulty facts) factor
A similarity factor (F2) is commonly described in drug dissolution testing area to reflect the similarity of two dissolution profiles by a number i.e. if the number is between 50 and 100 then the two profiles are considered similar. The question arises is in what respect are they similar; do numerically similar profiles show similar dissolution characteristics in the human GI tract- a commonly understood implication. No they do not, making this implication faulty. This is because the numbers are usually based on results obtained using apparatuses, and experimental conditions, which have never been qualified and validated for dissolution testing purposes. Therefore, similarity or dissimilarity of in vitro-in vivo profiles based on an F2 value has no meaning or relevance. Hence, presenting it as a useful parameter for bio-relevance is certainly a faulty fact.
It is often suggested, and in fact strongly promoted, that drug dissolution testing is a quality control tool, or an aid during the development of a product. This in itself is also a faulty fact. Drug dissolution testing by itself, without its in vivo link, has no meaning because both applications (QC and aid in product development) are derived from in vivo relevance, such as mandatory use of bio-relevant experimental conditions (e.g. 37 ºC, aqueous buffers etc.).
The similarity factor (F2) does not have any added value because a number between 50 and 100 reflects an average difference of dissolution 10% or less. Therefore, by definition, a quick way to establish similarity of the profiles is to calculate the average differences at different dissolution sampling times. If the value is less than 10% then, the curves meet the similarity (or F2) criteria. Derivation of the F2 value can often add biases and/or errors, e.g. one is restricted to use only one data point beyond 85% drug release. One is required to have two or more dissolution points to be able to calculate F2, however, a 10% difference would be easier to use and applicable irrespective to product type (fast release vs slow release) or the number of points/results available.
The range of 50 to 100 is not in line with current pharmacopeial requirements, even for QC purposes where a Q-based tolerance of 80% certainly allows a difference of 15 to 20% for products to have similar dissolution characteristics. However, F2 approach allows only differences of less than 10%.
Mathematically, the formula or calculations for the F2 does not appear to be more than a fancy skill testing question, such as “(2 × 4) + (10 × 3)” (Answer: 38) (link) or (8 x 6 – 5 + 9=52, link). The point being, it is a sort of arbitrary arithmetic exercise without any scientific relevance or value, however, it certainly adds burden on to the resources and interpretation.
In short, a similarity factor (F2) may be considered as not a very useful parameter which can lead to erroneous interpretation. The approach based on difference criteria (e.g. 10%) offers perhaps a simpler, logical and more robust approach for assessing the similarity or dissimilarity of the dissolution curves or results.
Confusion about IVIVC and predicting plasma drug levels
[As part of a discussion on the LinkedIn Network group (Pharmacokinetics), I posted the following response. For the interest of those who do not participate in the LinkedIn Network, or the particular group, I am posting the response on this blog as well. I hope that you will find the post useful.]
Thanks again Simon: [Simon’s post is attached at the end of my response]
I do not think we are going in circles, but in my opinion, you are either not following my point or avoiding it. Let me explain it another time.
“The aim of IVIVC is to Predict in vivo behavior from in vitro data.” This is incorrect. As the name (or “C”) implies, it is not a prediction exercise, but exercise in developing a correlation. For IVIVC, one has to have in vitro (i.e. dissolution) data as well as in vivo (plasma drug levels) data, and to relate them. No prediction what so ever.
Requirements and characteristics of performance verification test or tablets (PVT)
Before using any tester, it is commonly understood and often in fact is a requirement to establish that the tester is capable of measuring the expected parameter or characteristics. For our purpose, prior to its use, the apparatus or tester must be shown that it is capable of providing appropriate dissolution characteristics (i.e. percent drug dissolution at times) of a pharmaceutical product. There are different ways of saying the same thing, for example:
The tester is capable of measuring the dissolution characteristics with the required precision; the tester is fit for its intended purpose; or the tester is qualified and validated for its intended purpose.
A usual practice for establishing the “fit-for-purpose” or performance of a tester would be to determine dissolution characteristics, with its associated precision, of a reference product. If the tester provides the dissolution value, with required precision, then the tester will be considered as qualified and validated. Continue reading
Suggestions of developing and validating dissolution methods using compendial apparatuses, which are not qualified and validated, are simply promoting false science and useless practice!
The above title is self-explanatory, clear and says it all.
People have to be careful when offered help in developing and/or validating dissolution methods based on non-validated apparatuses (e.g. paddle/basket) and/or experimental conditions. The results obtained would not be of any use, even for QC purposes, no matter how they are presented.
The following links may be of further help in this regard. Continue reading
Why not obtain dissolution results from (slightly modified) assay and/or content uniformity testing? A simple and practical approach – Also, you will probably never need to develop and/or validate a dissolution method again.
For further details please see the following links:
- A Simple and Unique Approach for Developing and Evaluating Products (link)
- Assay and Content Uniformity (CU) based on dissolution testing (Poster Presentation). (link)
Some more relevant links:
- The science of drug dissolution testing: Testers or apparatuses, experimental conditions and interpretation of results – A systematic approach for learning. (link)
- Selecting a Dissolution Apparatus – Some Practical Considerations. (link)
- Drug Dissolution Testing Using Simple and Common Experimental Conditions (link)
- One Step (Product Evaluation) Approach (link)
- Can a dissolution test be used for assay and content uniformity testing? Of course! (link)
IVIVC (in vitro-in vivo correlation) – Time to let it go and move on!
An In-vitro in-vivo correlation (IVIVC) has been defined by the U.S. Food and Drug Administration (FDA) as “a predictive mathematical model describing the relationship between an in-vitro property of a dosage form and an in-vivo response”. For pharmaceutical products (tablets and capsules in particular) development purposes, in-vitro property and in vivo response mean in vitro drug dissolution/release characteristics and the plasma drug concentration profiles, respectively.
It is important to note that this relationship, or model, always exists between the two variables (dissolution vs plasma profile) for a given drug, which forms the basis for in vitro dissolution testing and its use for the assessment of quality of pharmaceutical products. Therefore, developing this relationship or modelling should have never been part of the practice of drug dissolution testing or its applications for products development or evaluation. However, this is precisely what has happened during the past two decades, i.e. repeated recommendations were made for correlating dissolution results with plasma drug levels. In fact, such developments have been suggested as regulatory requirements. Continue reading